Medical Cannabis | Opportunities and Obstacles
Despite prohibition and negative stigma over the past century, enthusiasm is growing for cannabis as a good treatment choice for many patients.
Dr Rosemary Mazanet | Chief Scientific Officer at Columbia Care
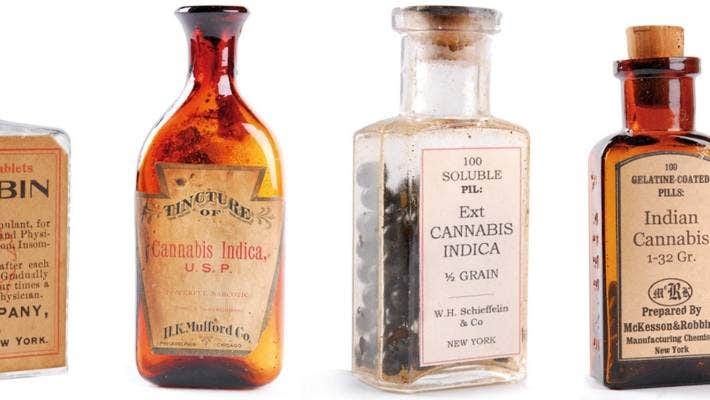
Despite prohibition and negative stigma over the past century, enthusiasm is growing for cannabis as a good treatment choice for many patients. In reality, cannabis has been used as a medicinal product for 5000 years to treat pain, nausea, anorexia, insomnia and convulsions. Cannabis-based medicines were sold in Europe and the US by early pharma companies until around 1930. Since that time, bad experiences with bootleg products and the idea that cannabis is solely recreational have clouded the public perception. Why are many physicians optimistic that new and diverse types of evidence will prove the benefits of cannabis based medicinal products (CBMPs) for appropriate patients? Nobody is claiming that CBMPs work for all patients and all conditions, but because the natural products from the cannabis plant cannot be patented like a pharmaceutical drug, it is unlikely that the cannabis industry will undertake expensive pharmaceutical type trials to provide that level of evidence. There needs to be a middle ground where medical professionals can define those disease states and symptoms where CBMPs are appropriate.

Underlying this argument is the firm scientific understanding of a mechanism of action explaining how phyto-cannabinoids (cannabinoids found in the plant) work in the body.
We know they act on the same cannabinoid receptors as the endocannabinoids that the body makes itself. The human endocannabinoid system (ECS) is comprised of receptors on cells throughout the body that are bound by natural endocannabinoids, or ingested phyto-cannabinoids, leading to biological downstream homeostatic effects. Endocannabinoids made by the body have been shown to exert positive effects in a number of disorders, including, musculoskeletal disorders and neurological disorders like epilepsy. Logically therefore, the effects of CBMPs are predicted by the distribution of the ECS receptors in the body. Cannabinoid Receptor-1 (CB1) is highly expressed in the brain and central nervous system (CNS), where it is involved with neurotransmitter release and impulse signalling. This might explain some activity of cannabis on mood disorders, motor disorders, and seizures. CB1 receptors are 10 times more prevalent in the brain and central nervous system than the μ-opioid receptor, which might explain the reduction in pain with CBMP use. Critically, CB1 receptors are not prevalent in the brainstem which may explain the lack of cannabis-related fatalities, unlike respiratory depression seen with morphine use. Cannabinoid receptor-2 (CB2) is more prevalent on blood cells, immune cells, and cells in muscle, spleen, liver and kidney, suggesting a role in anti-inflammatory modulation.
The cannabis plant contains many phyto-cannabinoids including the two most abundant, cannabidiol (CBD) and delta-9-tetrahydrocannbinol (THC). There are distinguishable difference in their effects, but when combined they have the potential to enhance the plant’s therapeutic benefits. CBD is also believed to balance out many undesired psychoactive activities of THC. For different conditions, the ratio of the respective phyto-cannabinoids in the CBMP required to achieve a pharmacologic effect may differ drastically, and therefore clinical research exploring this has been slow to emerge.
Because most endocannabinoids receptors are in the nervous system, is not surprising that a cannabis product (Epidiolex) gained marketing authorisation as a medicine for epilepsy syndromes.
Convincing clinical trials for other CNS-based conditions such as severe nausea from chemotherapy, and spasticity from multiple sclerosis has led to marketing authorisations for other CBMPs. There is abundant data indicating pain relief from neuropathic and other types of chronic pain with cannabinoids, but this does not come from one company financing a study focused on a single type of pain. This evidence comes from combined analysis of more than 2,500 patients in more than 29 randomised studies. Many governments and medical opinion leaders (including the National Institutes of Health and Drug Addiction in the USA) have stated publicly that these aggregate results, although derived from piecemeal trials, constitute convincing evidence for patient benefit and subsequently recommend cannabis use instead of opioids in some situations.
A very exciting prospect to help patients with poor treatment options exists for the CNS disorders of behaviour and mood, including opioid overuse.
Conditions such as autism, depression, PTSD and others remain poorly understood, and consequently effective treatments are lacking in current practice. Unfortunately, many of these patients are on an increasing cocktail of medicines, without discontinuing the previous ones, resulting in unpredictable drug combinations. There is an abundance of anecdotal cases describing where profoundly disabled patients, including children, were able to interact successfully with others and maintain improved behaviour after using CBMPs. Unfortunately, there has been a fear of using cannabinoid products in patients with these disorders as street-derived bootleg THC and cannabis based products mixed with other illegal psychogenic agents like “spice” or K2, have been implicated in increasing numbers of psychotic and bi-polar episodes. In light of this, CBMP research formulated under Home Office license is key and will hopefully dispel these fears.
The opioid crisis has forced the US and other countries to consider using cannabis instead of opioids for pain control. In view of the negligible risk of respiratory depression the increasing view that CBMPs are at least as “safe” as opioids is growing. Recent research has explored the potential for CBMPs in treating substance use disorders (a type of behaviour disorder) to help not only with any remaining pain symptoms, but also to reduce withdrawal symptoms and cravings. In a pilot trial in New York, 62% of patients who were taking opioids for neuropathic pain were able to reduce their opioid dosage in the year after they started using Columbia Care CBMPs. That study, funded by the US National Institute of Health, continues to collect and analyse the extracted longitudinal data. This was not a treatment trial but instead looked at patient utilisation data from existing health records. Nevertheless, it is valuable information.
What really constitutes convincing evidence for CBMP safety and efficacy? One could say that it depends on who is asking.
NICE may have a higher threshold for evidence than that of workplace NHS practice, such as treating neurology specialists. Animal studies are convincing but can only be relied on as preliminary evidence. Highly regulated MHRA or FDA quality scientific research with CBMPs will be unlikely due to the exorbitant costs. Longitudinal studies, like the one above with opioids, and registry data, where patients are tracked over time to see which products are used for what conditions, are therefore increasingly valuable, particularly if patients themselves are paying for the medicine. But the vote of the wallet is an unusual metric for the medical community to consider. Smaller trials, not looking for MHRA approval are warranted, and joint efforts by the health departments, academic institutions and interested physicians will be able to over time gather, digest and synthesise meaningful and diverse types data. Hopefully, we won’t need to wait another century.